High blood pressure: Don’t jump straight to medications
High blood pressure is a reading from 120-129 / 80 mmHg. Stage 1 hypertension is defined as a blood pressure of 130-140/80-90; Stage 2 >140/>90. Two readings gathered more than 8 weeks apart confirms the diagnosis. Many found problematic the 2017 ACC/AHA guideline that reclassified hypertension: “The prevalence of hypertension among US adults is substantially higher when the definition in the present guideline is used versus the JNC 7 definition (46% versus 32%)1.” Blood pressure is cyclical throughout the day, and many worried patients present to the ER with elevated numbers despite lack of symptoms. For a formidable but fascinating exposition of the “meaning of blood pressure,” see this article2. The 80 million US adults with hypertension are at risk for the most prevalent causes of death in the US (and the world), costing almost $50 billion annually3.
One high BP reading might not be reason to worry. But over many years, elevated blood pressure takes a toll on the vessels in your heart, kidneys, brain etc. Blood pressure control targets a “disease-oriented” outcome, albeit a very evidence-based one. For example, cholesterol studies often use LDL reduction as an outcome and claim success, but the intervention may not provide a mortality benefit. Healthcare professionals must consider “patient-oriented” outcomes both in clinical practice and in research4. Lowering the invisible molecule circulating in your bloodstream will not matter if you are disabled or dead. This doesn’t mean CRP, HDL, albumin and coronary blockages are not important, but doctors should consider the whole picture. Blood pressure does happen to be a pretty darn good surrogate / predictive outcome measure. Most of the studies cited below also evaluate claims on cardiovascular and overall morbidity and mortality.
This brief overview below abides by few rules: prioritization of clinical trials rather than retrospective studies, focus on causation over correlation, large sample sizes, and emphasis on systematic reviews and meta-analyses.
Diet
A rational approach to diet and lifestyle, with prioritization of circadian rhythm5, is paramount for most clinically relevant outcomes6,7. Follow the advice in the Perfect Health Diet8, to obtain most of your nutrients from a balanced, unprocessed, primal diet. Obtain as much protein as possible from cold water fish. Most experts believe the high omega 3 content improves many cardiovascular outcomes beyond blood pressure effects9. Shop at the grocery for a diverse selection of “superfoods”: nuts10, beets11, blueberries12, chocolate13, multiple14 teas15, and seaweed16 (also provides iodine). Consume foods high in magnesium (avocados, bananas, leafy greens, chocolate). Most people are subclinically deficient and should take a magnesium supplement17-19. Seek sources of vitamin K2 (grass-fed butter, hard cheeses, yolks, dark chicken, fermented soy), and dive into the evidence on K2 to reduce overall mortality20. Vitamin D has considerable effects on blood pressure, but is ideally obtained from the sun rather than a pill21.
Lifestyle
Reduce stress, give meditation a chance, even listening to music can reduce your blood pressure22,23. Weight loss in general24, and most forms of exercise25 have beneficial effects. Introduce a gratitude exercise26. Walk as often and as much as you can27, especially after a meal28.
Supplements
Several supplements with reasonable safety profiles appear to reduce blood pressure. Taurine has considerable evidence to reduce BP and minimal chance for adverse effects29-31. CoQ1032 and garlic33 have impressive data, both with favorable effects beyond blood pressure. Chen et al provide a description of numerous different herbal supplements that can help with blood pressure: L-arginine, chlorogenic acid, allicin from onions, soy and fish protein, ginkgo, theanine, and ginger14.
Conclusion
Of course, half of these research findings are false – who knows what future studies will find34. Nassim Taleb wisely argues that a historical framework of nutrition and fitness is more likely to remain accurate going forward35. Taleb also saliently addresses the iatrogenic effects of blood pressure medications, encouraging patients to adopt lifestyle changes they can stick with36. The human body is Antifragile37: just the right amount of stress (and just the right amount of blood pressure in our vessels) sends a signal that we better live longer or we will go extinct38. One of those healthy hormetic stressors is (intermittent) fasting itself, which of course has a role in blood pressure reduction, and researchers have some insight into the mechanisms39.
In summary, blood pressure (like everything else on earth) is cyclical40, so do not jump to conclusions when you see one high number. Visit an open-minded physician who will help you explore the impressive selection of lifestyle, diet, and supplement options before entering a long-term, dependent relationship with the pharmaceutical industry.
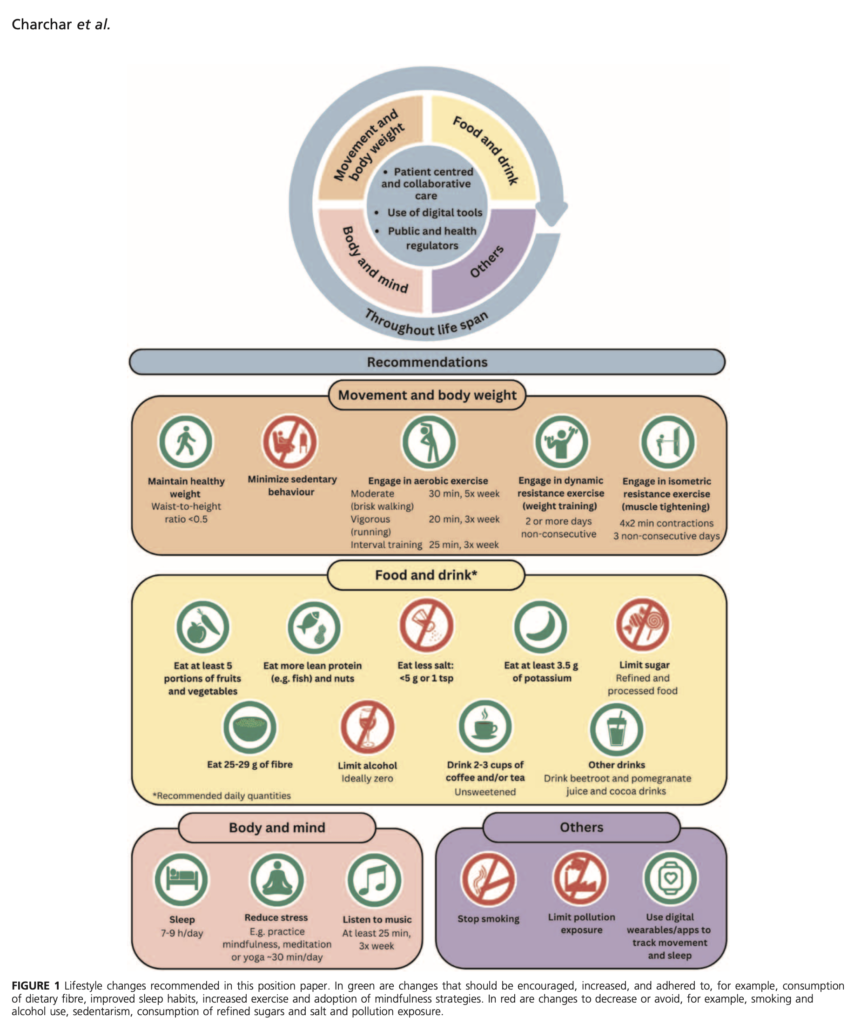
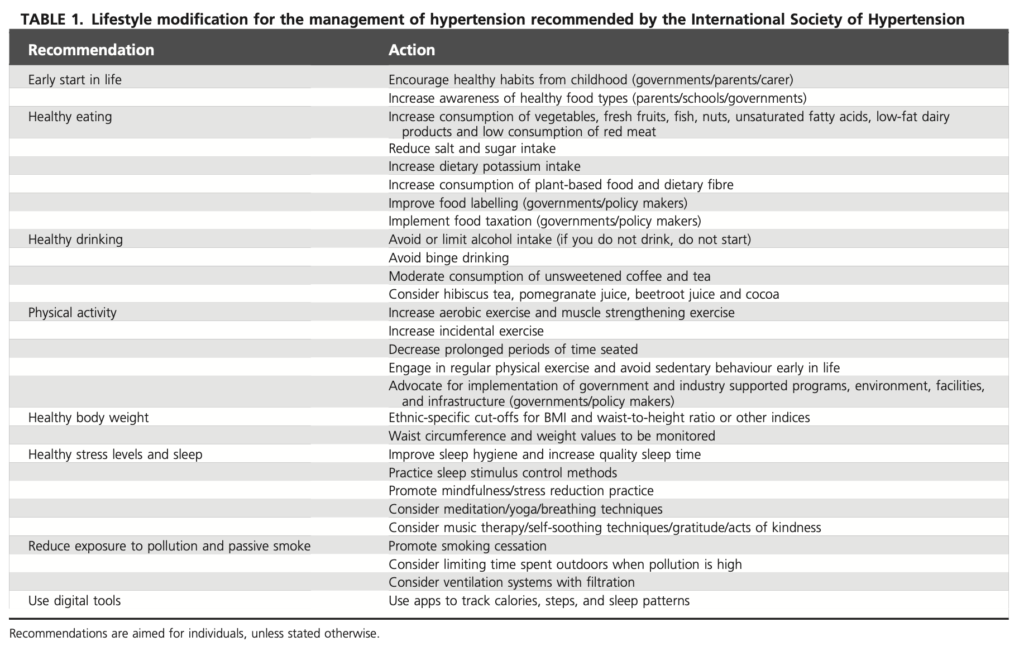
Here are two figures from a 2023 paper: Charchar, Fadi J.et al. Lifestyle management of hypertension: International Society of Hypertension position paper endorsed by the World Hypertension League and European Society of Hypertension. Journal of Hypertension. 2023. | DOI: 10.1097/HJH.0000000000003563
Reference List
1. Brook RD, Rajagopalan S. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Soc Hypertens. Mar 2018;12(3):238. doi:10.1016/j.jash.2018.01.004
2. Magder S. The meaning of blood pressure. Critical care. Oct 11 2018;22(1):257. doi:10.1186/s13054-018-2171-1
3. Writing Group M, Mozaffarian D, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. Jan 26 2016;133(4):e38-360. doi:10.1161/CIR.0000000000000350
4. de Grooth HJ, Parienti JJ, Oudemans-van Straaten HM. Should we rely on trials with disease- rather than patient-oriented endpoints? Intensive Care Med. Apr 2018;44(4):464-466. doi:10.1007/s00134-017-4859-0
5. Wang Y, Mei H, Jiang YR, et al. Relationship between Duration of Sleep and Hypertension in Adults: A Meta-Analysis. J Clin Sleep Med. Sep 15 2015;11(9):1047-56. doi:10.5664/jcsm.5024
6. Boers I, Muskiet FA, Berkelaar E, et al. Favourable effects of consuming a Palaeolithic-type diet on characteristics of the metabolic syndrome: a randomized controlled pilot-study. Lipids Health Dis. Oct 11 2014;13:160. doi:10.1186/1476-511X-13-160
7. Ghaedi E, Mohammadi M, Mohammadi H, et al. Effects of a Paleolithic Diet on Cardiovascular Disease Risk Factors: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Adv Nutr. Jul 1 2019;10(4):634-646. doi:10.1093/advances/nmz007
8. Jaminet P, Jaminet S-C. Perfect health diet : regain health and lose weight by eating the way you were meant to eat. 1st Scribner hardcover ed. Scribner; 2012:xx, 428 p.
9. Liu JC, Conklin SM, Manuck SB, Yao JK, Muldoon MF. Long-chain omega-3 fatty acids and blood pressure. Am J Hypertens. Oct 2011;24(10):1121-6. doi:10.1038/ajh.2011.120
10. Mohammadifard N, Salehi-Abargouei A, Salas-Salvado J, Guasch-Ferre M, Humphries K, Sarrafzadegan N. The effect of tree nut, peanut, and soy nut consumption on blood pressure: a systematic review and meta-analysis of randomized controlled clinical trials. Am J Clin Nutr. May 2015;101(5):966-82. doi:10.3945/ajcn.114.091595
11. Siervo M, Lara J, Ogbonmwan I, Mathers JC. Inorganic nitrate and beetroot juice supplementation reduces blood pressure in adults: a systematic review and meta-analysis. J Nutr. Jun 2013;143(6):818-26. doi:10.3945/jn.112.170233
12. Basu A, Du M, Leyva MJ, et al. Blueberries decrease cardiovascular risk factors in obese men and women with metabolic syndrome. J Nutr. Sep 2010;140(9):1582-7. doi:10.3945/jn.110.124701
13. Ried K, Sullivan TR, Fakler P, Frank OR, Stocks NP. Effect of cocoa on blood pressure. Cochrane Database Syst Rev. Aug 15 2012;(8):CD008893. doi:10.1002/14651858.CD008893.pub2
14. Chen ZY, Peng C, Jiao R, Wong YM, Yang N, Huang Y. Anti-hypertensive nutraceuticals and functional foods. J Agric Food Chem. Jun 10 2009;57(11):4485-99. doi:10.1021/jf900803r
15. McKay DL, Chen CY, Saltzman E, Blumberg JB. Hibiscus sabdariffa L. tea (tisane) lowers blood pressure in prehypertensive and mildly hypertensive adults. J Nutr. Feb 2010;140(2):298-303. doi:10.3945/jn.109.115097
16. Teas J, Baldeon ME, Chiriboga DE, Davis JR, Sarries AJ, Braverman LE. Could dietary seaweed reverse the metabolic syndrome? Asia Pac J Clin Nutr. 2009;18(2):145-54.
17. DiNicolantonio JJ, O’Keefe JH, Wilson W. Subclinical magnesium deficiency: a principal driver of cardiovascular disease and a public health crisis. Open Heart. 2018;5(1):e000668. doi:10.1136/openhrt-2017-000668
18. Reffelmann T, Ittermann T, Dorr M, et al. Low serum magnesium concentrations predict cardiovascular and all-cause mortality. Atherosclerosis. Nov 2011;219(1):280-4. doi:10.1016/j.atherosclerosis.2011.05.038
19. Zhang X, Li Y, Del Gobbo LC, et al. Effects of Magnesium Supplementation on Blood Pressure: A Meta-Analysis of Randomized Double-Blind Placebo-Controlled Trials. Hypertension. Aug 2016;68(2):324-33. doi:10.1161/HYPERTENSIONAHA.116.07664
20. Juanola-Falgarona M, Salas-Salvado J, Martinez-Gonzalez MA, et al. Dietary intake of vitamin K is inversely associated with mortality risk. J Nutr. May 2014;144(5):743-50. doi:10.3945/jn.113.187740
21. Mozaffari-Khosravi H, Loloei S, Mirjalili MR, Barzegar K. The effect of vitamin D supplementation on blood pressure in patients with elevated blood pressure and vitamin D deficiency: a randomized, double-blind, placebo-controlled trial. Blood Press Monit. Apr 2015;20(2):83-91. doi:10.1097/MBP.0000000000000091
22. do Amaral MA, Neto MG, de Queiroz JG, Martins-Filho PR, Saquetto MB, Oliveira Carvalho V. Effect of music therapy on blood pressure of individuals with hypertension: A systematic review and Meta-analysis. Int J Cardiol. Jul 1 2016;214:461-4. doi:10.1016/j.ijcard.2016.03.197
23. Nidich SI, Rainforth MV, Haaga DA, et al. A randomized controlled trial on effects of the Transcendental Meditation program on blood pressure, psychological distress, and coping in young adults. Am J Hypertens. Dec 2009;22(12):1326-31. doi:10.1038/ajh.2009.184
24. Semlitsch T, Jeitler K, Berghold A, et al. Long-term effects of weight-reducing diets in people with hypertension. Cochrane Database Syst Rev. Mar 2 2016;3:CD008274. doi:10.1002/14651858.CD008274.pub3
25. Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. Feb 1 2013;2(1):e004473. doi:10.1161/JAHA.112.004473
26. Jackowska M, Brown J, Ronaldson A, Steptoe A. The impact of a brief gratitude intervention on subjective well-being, biology and sleep. J Health Psychol. Oct 2016;21(10):2207-17. doi:10.1177/1359105315572455
27. Mandini S, Conconi F, Mori E, Myers J, Grazzi G, Mazzoni G. Walking and hypertension: greater reductions in subjects with higher baseline systolic blood pressure following six months of guided walking. PeerJ. 2018;6:e5471. doi:10.7717/peerj.5471
28. Diekmann C, Wagner M, Huber H, et al. Acute Impact of Dietary Pattern and Walking on Postprandial Attention, Mood, and Satiety in Older Adults: A Randomized Crossover Trial. Nutrients. Sep 26 2019;11(10)doi:10.3390/nu11102294
29. Guan L, Miao P. The effects of taurine supplementation on obesity, blood pressure and lipid profile: A meta-analysis of randomized controlled trials. Eur J Pharmacol. Oct 15 2020;885:173533. doi:10.1016/j.ejphar.2020.173533
30. Shao A, Hathcock JN. Risk assessment for the amino acids taurine, L-glutamine and L-arginine. Regul Toxicol Pharmacol. Apr 2008;50(3):376-99. doi:10.1016/j.yrtph.2008.01.004
31. Sun Q, Wang B, Li Y, et al. Taurine Supplementation Lowers Blood Pressure and Improves Vascular Function in Prehypertension: Randomized, Double-Blind, Placebo-Controlled Study. Hypertension. Mar 2016;67(3):541-9. doi:10.1161/HYPERTENSIONAHA.115.06624
32. Rosenfeldt FL, Haas SJ, Krum H, et al. Coenzyme Q10 in the treatment of hypertension: a meta-analysis of the clinical trials. J Hum Hypertens. Apr 2007;21(4):297-306. doi:10.1038/sj.jhh.1002138
33. Reinhart KM, Coleman CI, Teevan C, Vachhani P, White CM. Effects of garlic on blood pressure in patients with and without systolic hypertension: a meta-analysis. Ann Pharmacother. Dec 2008;42(12):1766-71. doi:10.1345/aph.1L319
34. Ioannidis JP. Why most published research findings are false. PLoS Med. Aug 2005;2(8):e124. doi:10.1371/journal.pmed.0020124
35. Lieberman D. The story of the human body : evolution, health, and disease. First edition. ed. Pantheon Books; 2013:xii, 460 pages.
36. Clear J. Atomic habits : tiny changes, remarkable results : an easy & proven way to build good habits & break bad ones. Avery, an imprint of Penguin Random House; 2018:ix, 306 pages.
37. Taleb NN. Antifragile : things that gain from disorder. 1st ed. Random House; 2012:xxi, 519 p.
38. Calabrese EJ, Agathokleous E. Building Biological Shields via Hormesis. Trends Pharmacol Sci. Jan 2019;40(1):8-10. doi:10.1016/j.tips.2018.10.010
39. Camelo L, Marinho TS, Aguila MB, Souza-Mello V, Barbosa-da-Silva S. Intermittent fasting exerts beneficial metabolic effects on blood pressure and cardiac structure by modulating local renin-angiotensin system in the heart of mice fed high-fat or high-fructose diets. Nutr Res. Mar 2019;63:51-62. doi:10.1016/j.nutres.2018.12.005
40. Field JM, Bonsall MB. The evolution of sleep is inevitable in a periodic world. PloS one. 2018;13(8):e0201615. doi:10.1371/journal.pone.0201615
